Abstract
Introduction:
Diffuse Large B Cell Lymphoma (DLBCL) is an aggressive lymphoma with a heterogeneous clinical, histological, immunophenotypic and cytogenetic features that translate into variable prognosis. The Rituximab-International Prognostic Index (R-IPI) score considers patient´s and tumor´s characteristics and identifies 3 prognostic groups. However among patients in the same risk group, outcomes are diverse, even with the use of modern immunochemotherapy regimens and there is a subgroup of patients with a 5-year overall survival (OS) probability of less than 50%.
Therefore, the recognition of prognostic biomarkers capable to better stratify patient´s risk has been the focus of extense research, and identifying cheap, easily available and simple tools seems a valious goal. Monocytes act as host anti-tumor immunity suppressors and as promoters of malignant lymphocyte´s growth and survival and there is evidence that elevated absolute monocyte count (AMC) is independently associated with inferior PFS and OS in patients with DLBCL. The objective of this study is to evaluate the prognostic value of the AMC at diagnosis in our population of patients with DLBCL treated with chemoimmunotherapy.
Materials and Methods:
Retrospective analysis of 202 patients with newly diagnosed DLBCL between 2002 and 2017 treated at Hospital de Clínicas and Hospital Maciel, the two main health public reference services in Montevideo-Uruguay.
AMC was determined from routine automated complete blood count (CBC) at diagnosis, prior to therapy administration. The cut off value considered for AMC was 630/mm3, according to Wilcox et al. Leukemia (2011) 25, 1502-1509. Treatment response was defined according to the International Workshop criteria. This study complied with all provisions of the Declaration of Helsinki and its current amendments and was conducted in accordance with Good Clinical Practice Guidelines.
Results:
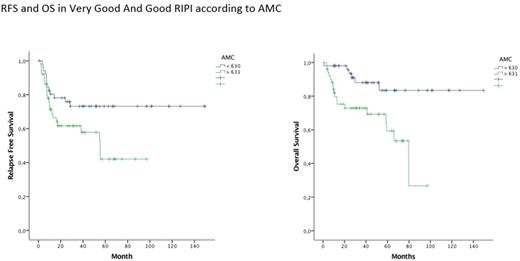
Among the entire population, 177 patients received immunochemotherapy (R-CHOP or R-CHOP like) with a median of rituximab cycles of 6 (1-6). Median age was 61 (17-85); 99 (56%) were female; 74 patients (42%) had stage I-II, 103 (58%) stage III-IV. According to RIPI score; 10 (5,6%) had very good prognosis, 97 (54,8%) good prognosis and 70 (39,6%) adverse prognosis. Four percent were HIV positive. Median AMC at diagnosis was 620 (40-3720). At the end of treatment 118 patients (66,7%) achieved Complete Remission (CR). Forty percent were refractory or relapsed. According to AMC, CR rates were 63% when AMC was ≥ 631/mm3 and 71,8% with AMC < 631/mm3 (p=0,25) There was no difference in the median cycles of rituximab among these groups. When grouped according to RIPI score, AMC was associated with different RC rates. In very good and good RIPI score (0-2) CR was 80,8% in AMC <631/mm3 and 62,7% in AMC ≥ 631/mm3 (p=0,042). No difference was found in CR among adverse RIPI score according to AMC (57,6% vs 64,7% p=0,54). With a median follow up of 27,8 months (0,6-149) median OS in the group of patients with high AMC was 79,7 months (47-112) vs 131 months (20,6-242,6) in low AMC (p=0,016) This population was comparable in terms of RIPI score. In the subgroup of patients with very good and good RIPI the median OS in patients with low AMC has not been reached and was 79,7 months in high AMC (55,7-103,8 p=0,002). There was no statistically significant difference in median OS in patients with adverse RIPI score according to AMC (131 vs 101 months p=0,94). The Relapse Free Survival (RFS) among RIPI 0-2 was not reached in those with low AMC and was 55 months (35,7-74-8) with high AMC (p=0,039)
In high risk RIPI patients, there was no difference in RFS among both groups (16,7 months vs 28,1 p=0,58). No significant difference was found in RFS and OS when patients with RIPI 0-2 with high AMC were compared to those with RIPI 3-5 (55 vs 28 months p= 0,55 and 79,7 vs 101 months p=0,82 respectively)
Discussion:
Outcome of patients with DLBCL is variable even among the same prognostic group according to traditional scores. In our study high AMC was associated with inferior CR rates, RFS and OS. This difference was statistically significant in very good or good prognosis RIPI and patients in this group with high AMC had similar OS than adverse prognostic RIPI patients. This results suggest that a low cost and accessible test as AMC could improve prognostication of patients with DLBCL, particularly in the group of good prognosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal